Mesenchymal stem cells demonstrate remarkable potential in the field of regenerative medicine. These multipotent mesenchymal cells are capable of differentiate into a variety of cell types, including bone, cartilage, and muscle. Transplantation of mesenchymal stem cells to damaged tissues has shown promising results in repairing a wide range of conditions, such as neurodegenerative disorders, diabetes, and autoimmune diseases.
These cells exert their therapeutic effects through various mechanisms, including direct cell replacement, signaling factor release, and modulation of the immune system. Future research is directed on optimizing mesenchymal stem cell transplantation protocols to enhance success rates.
Stem Cell Injections: A Novel Approach to Tissue Repair
Stem cell administration have emerged as a promising approach for tissue regeneration. These specialized cells possess the remarkable ability to differentiate into various cell types, offering a potential therapy for a wide range of degenerative diseases. By implanting stem cells into damaged tissues, researchers aim to stimulate the body's inherent healing processes.
The clinical potential of stem cell injections spans a diverse spectrum of conditions, including cardiac diseases. Pre-clinical studies have shown positive results, suggesting that stem cells can enhance tissue function and reduce symptoms.
Investigating the Therapeutic Potential of Induced Pluripotent Stem Cells
Induced pluripotent stem cells (iPSCs) possess a groundbreaking avenue for medical interventions due to their remarkable ability to differentiate into diverse cell types. These cells, obtained from adult somatic cells, are reprogrammed to an embryonic-like state through the introduction of specific transcription factors. This reprogramming enables scientists to produce patient-specific cell models for disease modeling and drug evaluation. Furthermore, iPSCs hold immense opportunity for restorative medicine, with applications in reconstructing damaged tissues and organs.
Autologous Stem Cell Injection in Osteoarthritis: A Clinical Review
Osteoarthritis presents a significant public health concern, marked by progressive cartilage degradation and joint dysfunction. Autologous stem cell transplantation has emerged as a novel therapeutic strategy for alleviating osteoarthritis symptoms. This overview examines the current knowledge regarding autologous stem cell transplantation in osteoarthritis, assessing its efficacy and drawbacks. Recent research suggests that autologous stem cells may contribute in mitigating cartilage damage, reducing pain and inflammation, and improving joint function.
- Despite this, further research are required to establish the long-term safety and best protocols for autologous stem cell transplantation in osteoarthritis.
- Upcoming research should focus on targeting specific patient populations most likely to benefit from this intervention and refining delivery methods for enhanced clinical outcomes.
Understanding the Impact of Stem Cell Homing and Engraftment on Treatment Outcomes
The efficacy/effectiveness/success of stem cell-based therapies hinges critically on the ability of transplanted cells to migrate/localize/home to the target tissue/intended site/designated region and integrate/engrafted/become established. This process, known as homing and engraftment, involves a complex interplay of cellular signaling pathways/molecular cues/biological mechanisms that guide stem cell movement and their subsequent proliferation/survival/differentiation within the recipient environment/niche/microclimate.
Successful homing and engraftment are essential for therapeutic benefit/positive clinical outcomes/disease modification, as they allow transplanted cells to replace damaged tissues/restore lost function/mediate tissue repair. Factors influencing this process include the type of stem cell/source of stem cells/specific stem cell population used, the nature of the disease/underlying condition/health status being treated, and the delivery method/transplantation technique/administration strategy employed.
Researchers/Scientists/Clinicians are actively investigating strategies to enhance homing and engraftment to improve treatment outcomes/for better clinical efficacy/to maximize therapeutic potential. This includes exploring bioengineered scaffolds/pharmacological agents/genetic modifications that can promote cell migration/facilitate cell integration/enhance survival of transplanted cells.
Ethical Considerations in Stem Cell Injection Therapies
Stem cell injection treatments hold immense possibilities for repairing damaged tissues and organs. However, the burgeoning field of stem cell medicine raises a number of complex click here ethical dilemmas. One key concern is the efficacy of these approaches, as research are ongoing. There are also worries about the source of stem cells, particularly regarding the harvesting of embryonic stem cells. Furthermore, the price of stem cell therapies can be prohibitive, raising questions about equity to these potentially life-changing therapies. It is essential that we contemplate these ethical considerations carefully to ensure the moral development and use of stem cell therapies for the well-being of humanity.
 Patrick Renna Then & Now!
Patrick Renna Then & Now! Andrea Barber Then & Now!
Andrea Barber Then & Now! Heather Locklear Then & Now!
Heather Locklear Then & Now! Barbara Eden Then & Now!
Barbara Eden Then & Now!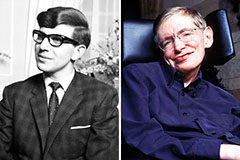 Stephen Hawking Then & Now!
Stephen Hawking Then & Now!